












          |
   |
|
|
“AESOP, IN! AESOP, DOWN!” That’s not the sound of someone shouting commands to their pet, it’s one of the phrases W. Clark Hargrove III, M.D., uses while performing mitral valve surgery.
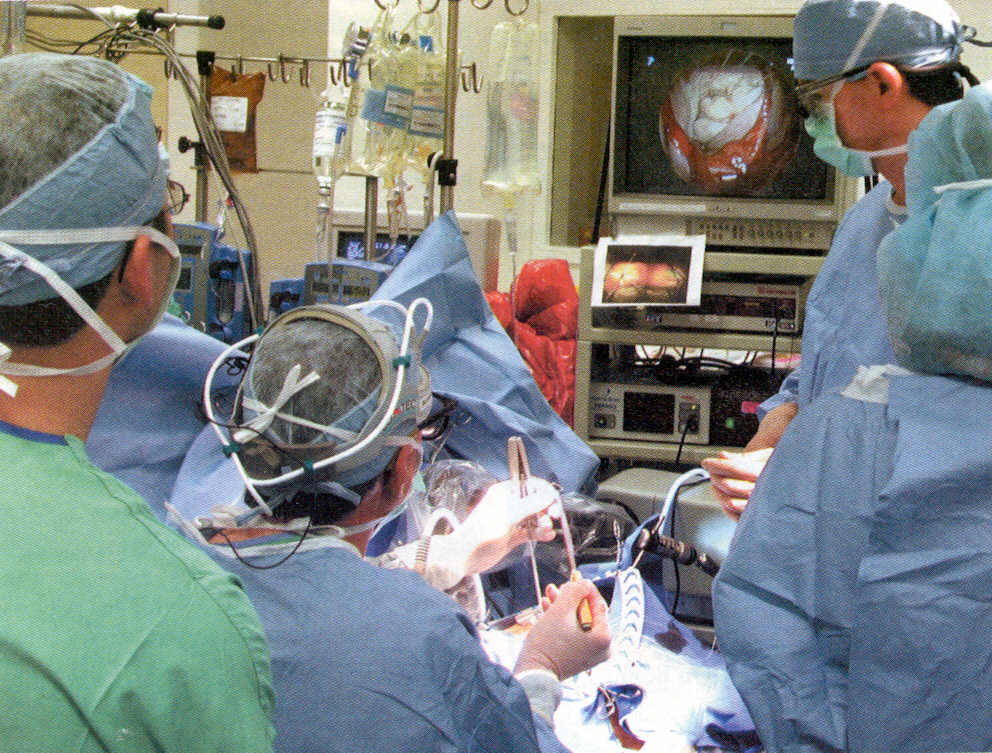
Hargrove, Clinical Director of Cardiothoracic Surgery at Presbyterian Medical Center and renowned for his skill in mitral valve repair and replacement, is talking to AESOP 7, a robotic arm that holds an endoscope containing a tiny camera. AESOP (Automated Endoscopic System for Optimal Positioning) is electronically programmed to instantaneously respond to Hargrove’s voice and when the surgeon wants to peer into a heart’s interior during an intricate mitral valve operation, he uses clipped commands to instruct the robot to change positions. The video images from the robotic endoscope are displayed on a monitor adjacent to the operating table, providing Hargrove - and his entire OR team - with a bird’s eye view of the patient’s mitral valve. This sophisticated robotic system is revolutionizing cardiac surgery
”Before AESOP, a resident who was assisting in an operation couldn't really get a good look at what I was doing, but now he or she can look at the video screen and see exactly how I'm going to fix a mitral valve," Hargrove says. “The principles of surgery haven’t changed, but our technology certainly has.” Using long-handled surgical tools and watching his own movements on the video screen, Hargrove performs delicate mitral valves repairs and replacements through small incisions in the patient's chest. Because he watches the heart on a video screen instead of looking inside the patient’s body, Hargrove is able to reduce the size of the incisions he makes in the chest. Smaller incisions translate into dramatically reduced trauma and quicker recovery for patients. “Because of the picture the endoscope provides, we only need a three inch incision to see what used to require a five inch incision during minimally invasive surgery,” Hargrove explains.
The AESOP robotic arm is the first surgical robot approved by the United States Food and Drug Administration. Presbyterian Medical Center is currently the only facility in the region to use AESOP during cardiac surgery. While the presence of a robotic device in an operating room seems downright futuristic, Hargrove considers it an amazing yet natural progression in the art of cardiac surgery. “The use of robots ushers us into a new age of cardiothoracic surgery, and AESOP represents one of the initial steps in an evolutionary process,” Hargrove says. Minimally invasive surgery was the first step in revolutionizing cardiac procedures. Instead of performing a sternotomy (which involves cutting the chest and pulling the ribs apart to gain access to the heart), minimally invasive surgery involves small incisions through which the surgeon operates under direct vision.
AESOP’s video-assisted heart surgery takes minimally invasive mitral valve operations to a new level, providing Hargrove with a “secondary vision”when the endoscope that is placed through an incision projects exceptionally clear images of the patient's heart onto a high-quality screen, thus eliminating or limiting the need for direct vision. While its robotic arm holds the endoscope with a steadiness that no human can match, AESOP provides Hargrove with detailed views of the heart during surgery, which is a definite advantage when working on mitral valves.
“The mitral valve is a complex structure, shaped somewhat like a parachute. When we used sternotomy, we had to approach the mitral valve in the middle, but with AESOP, the camera comes in from the patient's right side and we see the entire valve in its natural environment,” Hargrove says. “You get a better view of the mitral valve because you can instruct the robotic camera to go right down inside of the ventricular cavity.”
Jeanne Fox, RN, MSN, CRNP, reports that AESOP is still experimental and has only been approved by the U.S. FDA with open-chest procedures with mitral valve surgery. Ms. Fox points out that, in addition to better visualization of the mitral valve, there are other distinct advantages. “With AESOP, the patient still needs to go on heart bypass but there is only a 3-inch incision made under the right breast to allow for passage of the endoscopic robot arm. With the smaller incision, there is less pain and quicker return to daily activities.” Ms. Fox is the cardiothoracic nurse practitioner. She works closely with Hargrove and is the primary patient liaison for all heart surgery patients and their families.
The mitral valve is situated in the heart’s interior, so the organ must remain still during mitral valve repair or replacement. Patients are placed on cardiopulmonary bypass machine to stop the beating of their heart and to artificially pump blood through their body during mitral valve surgery. (In the future, surgeons hope to evolve towards video assisted, beating heart coronary surgery.)
Hargrove notes that it takes intense training and years of surgical experience to operate AESOP and other robotic technology systems. “A robot is only as smart as the person running it, and you have to move through a step-wise progression to perfect the technique,” Hargrove says. “A surgeon I know compares it to climbing Mt. Everest. He says you can't reach the top on the first day- you start at base camp one, and then gradually progress to the summit.”
The goal at Presbyterian is to progress to total port cardiovascular surgery. Using this amazing technique, instead of manipulating the patient directly, the surgeon views the patient’s heart on a video monitor and operates through robotic instruments that he or she controls while seated at a nearby console (located either in the operating room or in another room). With the aid of a computer, the surgeon’s actions at the remote console are replicated by robotic arms that have surgical instruments attached. The robot performs the surgical movements with the precision that increasingly advanced minimally invasive procedures demand. Using this space-age technology, the surgeon will be able to orchestrate complex procedures that are currently impossible to perform.
Hargrove says that, theoretically, if robotic surgeries become standardized, surgeons could perform total port surgery on a patient who is in another hospital – or even another country. “Before the advent of computers, we never dreamed that we could look at an X-ray of a patient in New York while sitting in our offices in Philadelphia, so you just never know what's next. This current technology is unbelievable,” says Hargrove. “Five years ago, cardiac surgery seemed like a mature specialty, but we are now on the threshold of new discoveries.” Hargrove says that Harvey Waxman, M.D., Chief of Cardiology at Presbyterian, was vigilant about bringing the AESOP system to the medical center. And although he is cautious about predicating the future of robotics in the operating room - as befits a man of science - Hargrove has no doubts about AESOP's contribution to cardiac surgery.
“If I needed mitral valve surgery, it’s the way I’d have mine done, which is usually the barometer I use,” he says with a smile. “The important aspect of this technique is that we can now accomplish anything that we used to using sternotomy, yet patients enjoy a shorter hospital stay, less post-operative pain, and a quicker return to daily function, which saves stress, time and money for everyone involved.”
Grateful acknowledgment to the Presbyterian Medical Center of the University of Pennsylvania Health System for contributing this page
Articles |
Newsletters |
Recipes |
Women's Stories |
Press Releases |
Wellness Calendar
Back to top
Disclaimer | Donate Now | Contact Us | Site Map | Store
|
©1999-2000; updates: 2002, 2004, 2005, 2007 Women's Heart Foundation, Inc. All rights reserved. Unauthorized use prohibited. The information contained in this Women's Heart Foundation (WHF) Web site is not a substitute for medical advice or treatment, and WHF recommends consultation with your doctor or health care professional. |